The following dispatch was sent by a nurse who asked to remain anonymous in order to protect their job.
The state I live in would be classified as having a high rural population, and I work for a hospital that is struggling financially and part of large nationwide health system. We have had no communication from the top of our organization. This leads me to believe that they have no idea how to handle this situation, and my local administration has no idea how to handle this either.
The first I heard any communication from anyone about precautions for coronavirus were small, colored signs asking patients and visitors to “Stop! If you have cough, fever … or have traveled outside the US or had contact with someone that has.” I am trying to quote the sign, but it’s from memory. These were posted right around the time we had the first confirmed case of coronavirus in the U.S. Up until this sign was placed, the only person I had heard mention coronavirus was one of the guys in Supply Chain who was irked that Personal Protective Equipment (PPE) was on back order due to what was going on in China.
The next communication we had was in the form of e-mail. It might surprise most people, but e-mail is a terrible way to communicate to patient caregivers. While plenty of nurses sit in front of a computer, they are rarely logged onto e-mail — they are charting medical documentation on their patients. Nurses, like all the other staff in the hospital that has actual physical contact with patients regularly, do not routinely check their e-mails. They simply are too busy with patient care activities to remember to log in and get the latest newsletter the hospital sends out. Any updates or changes to protocols or policy will reach these staff members long after they have been announced because the information will trickle down to them in an incredibly inefficient game of telephone. The first e-mail was sent out on March 5. It instructed staff that if they happened across a patient they suspected needed to be tested for coronavirus, that we should place a regular mask on the patient, stay six feet away, and contact a Charge RN who would have the appropriate training to handle the situation.
Every healthcare worker should know, and sadly there are probably many that don’t, that PPE gear isn’t used this way. The masks they want us to place on the patient are loose fitting. The air patients breathe out will just go out the sides of the mask. If a patient is already infected, these masks will do next to nothing to prevent an airborne virus.
The next update to our coronavirus policy came on March 9. It stated that we will most likely end up treating one of these patients in the future. This update was to remind us that we had to keep patient privacy in mind and that we need to not discuss patients on social media or outside the hospital. This e-mail showed a clear misunderstanding of what the coronavirus even is. If you treat one patient, you will be treating more. It was becoming alarming that leadership in my hospital — leadership that includes physicians — were not understanding the potential severity of an outbreak.
Next update was March 11. These other e-mails were from lower-level people in administration. Secretaries sending out a quick note from their bosses. This e-mail was the first that we got from our Top Physician Administrator. We are thanked for our hard work and are assured that we are fully prepared to handle patients with Covid-19. We are told that they are following the CDC recommendations and that the risk according to the CDC is low. A few brief statements about how we need to practice good hygiene, isolation precautions, and that they are working with the local health department. The bulk of this e-mail is regarding privacy. I quote:
In cases where patients have tested positive for coronavirus, the name of the facility treating the patient is not publicly disclosed. We respect and honor that decision. As we receive these patients, their information and diagnosis will remain confidential; we will not be making any public statement about COVID-19 to protect patient privacy.
This is NOT about patient privacy. This is about keeping the doors open for routine business and not hoping that this silly, inconvenient virus doesn’t impact their bottom line too much. I keep reading about how bad things are in Italy, how hardly anyone in the U.S. is getting tested, and I’m really starting to worry that we are going to be overwhelmed. We aren’t slowing down elective procedures, we aren’t trying to empty our ICUs to be prepared, we aren’t designating an area where suspected patients will be placed to limit exposure, we aren’t limiting the number of visitors allowed. We did put up a larger version of the original sign, so that should keep the virus out…Next update was March 11. A few brief statements about how we need to practice good hygiene, isolation precautions, and that they are working with the local health department.
Next update is March 12. We are now only allowing two patient visitors in the hospital per day. We have also suspended our volunteer programs since most of our volunteers are elderly. We finally get information from the top physician of our nationwide health system. He says, “With insight from our sister —– hospitals in other states experiencing outbreaks of COVID-19, we decided to make these changes out on an abundance of caution.”
Next update March 13. (Can you see how the panic and worry is starting to build?) They finally call it a pandemic!! They are now asking staff to voluntarily report any upcoming travel plans. They are not planning to restrict return to work after travel, but they state that this could change. They warn especially against cruises.
Friday was the first day that I got to see my hospital’s response to our first potential coronavirus patients. Our hospital was expecting to receive a patient in respiratory distress that had arrested, but we got a panicked phone call from someone — either from the transferring hospital or someone from EMS that would be doing the transporting. This individual wanted to divert the patient to another hospital because they heard we had positive coronavirus patients. Management was furious, and told them that of course we have suspects, but no one has been confirmed positive yet, and says that the patient is safe to be transferred here. The incoming patient was to be placed in a regular Intensive Care Unit — alongside all the other ICU patients that are not potential coronavirus patients.
Late afternoon a coworker tells me of an incident that occurred in another one of our ICU areas. A tech was supposed to perform a test on a patient in this ICU. There are no signs, there is no isolation gear available. The Tech goes on about their business because there are no warnings in place. They enter the patient’s room and introduce themselves and explain what they are doing there. The patient is hard of hearing. The tech, in order to communicate to the patient, gets closer to the patient’s face, roughly eye level — which means they are nose to nose and mouth to mouth level as well — when the tech is pulled away by the patient’s nurse and ushered outside the room. They are then told by this nurse that this patient is a potential coronavirus patient. The tech immediately questions why there weren’t any signs on the patient’s door. The nurse tells the tech that they were instructed not to hang signs in order to avoid a panic. The tech is not sent home and is expected to continue working. The only thing that will change is that they must wear a standard mask — the one that vents air out of the sides.
Another incident. One of my very close friends has a job where he takes care of a special patient population with a certain medical condition. These are very sick people who require a team of individuals to care for them and he rounds with the physician and the other care team members daily on these patients when they are admitted to the hospital. I called him to tell him about the Tech situation and to complain about how bad administration is making the situation and he then tells me that he has been exposed.
On Thursday, he and his team members performed their daily rounding on one of their patients. That afternoon a family member visited this patient. The entire team rounds on the patient on Friday morning. They are then later informed by the patient’s floor nurse that the family member who visited on Thursday afternoon has been in direct contact with the husband/wife of the first positive Covid-19 patient identified in my state. This patient remains in the same unit — not an intensive care unit — and has been placed on Contact Precautions. Contact Precautions are not the same as Airborne Precautions. It’s something, but does not fully address coronavirus protections. Why the physicians and administrators of my hospital can’t make this distinction is something that alarms and baffles me.
This is the problem. This is two days, and these are the only the examples I have heard of. We have been set up for failure and the measures we are taking will only spread this infection, not limit it. Patients having elective procedures need to cancel. We need to stop elective surgeries to free up ventilators. We need to start considering turning operating rooms into holding areas for all our potential patients.
At first, I was worried that we might have it half as bad as Italy. I can tell you from what I have now witnessed, we are Italy.
Thanks for your time.
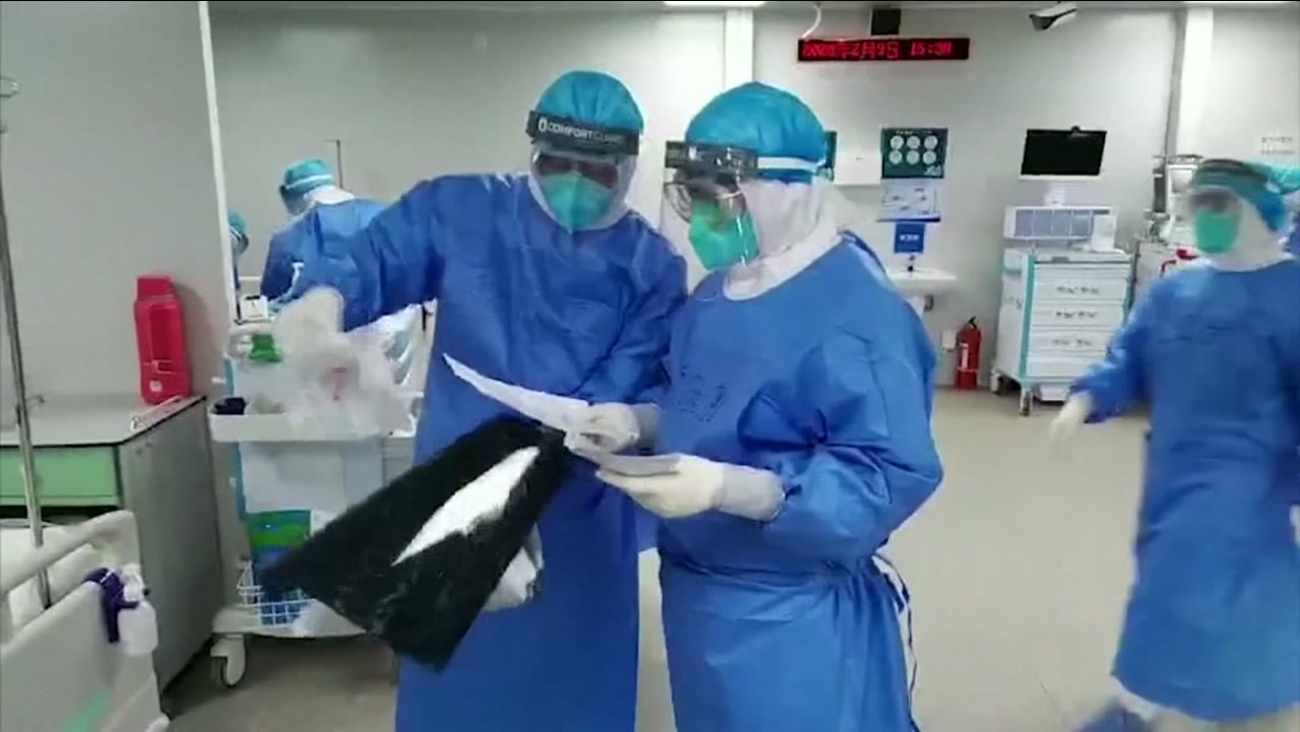
Meanwhile, the biggest victim of this pandemic has sent its experienced health workers to the Italian COVID-19 frontlines, in order to help the country during its time of need.

